Navigating the intricacies of maintaining insurance coverage during long-term disability can be a complex and often daunting task.
For many individuals, the sudden shift from regular employment to long-term disability brings with it a host of questions, particularly regarding the continuity of their health coverage.
Understanding who is responsible for covering these costs during such a challenging period is crucial for financial planning and ensuring uninterrupted access to necessary medical care.
The Role of Employer-Provided Benefits
Typically, in many employment scenarios, employers provide health insurance as part of their benefits package. When an employee transitions to long-term disability, the specifics of this coverage can vary significantly based on the employer’s policies and the terms of the insurance plan.
Some employers may continue to pay the premium for a set period, while others might require the employee to take over the payment. It’s essential for employees to review their employer’s disability policy and the health insurance plan to understand the terms of coverage during long-term disability.
This information is usually outlined in the employee benefits handbook or can be obtained from the human resources department. In some cases, the continuation of coverage might depend on the length of employment or other specific criteria set by the employer.
Government Programs and Their Scope
In certain jurisdictions, government programs can provide relief for those on long-term disability. Programs like Medicare in the United States may become available to individuals after they have been on Social Security Disability Insurance (SSDI) for a specific period (usually 24 months).
For younger individuals or those not qualifying for Medicare, exploring options under the Affordable Care Act (ACA) might be beneficial. The ACA provides avenues to purchase insurance through marketplaces, often with subsidies available based on income levels, which can be particularly helpful when one’s income is reduced due to disability.
What’s Its Role?
Those who have private disability insurance policies need to review their policy details. Some private disability plans offer provisions to cover health insurance premiums, but this is not universally the case. Policyholders should contact their insurance provider to clarify the terms and conditions related to health coverage during long-term disability.
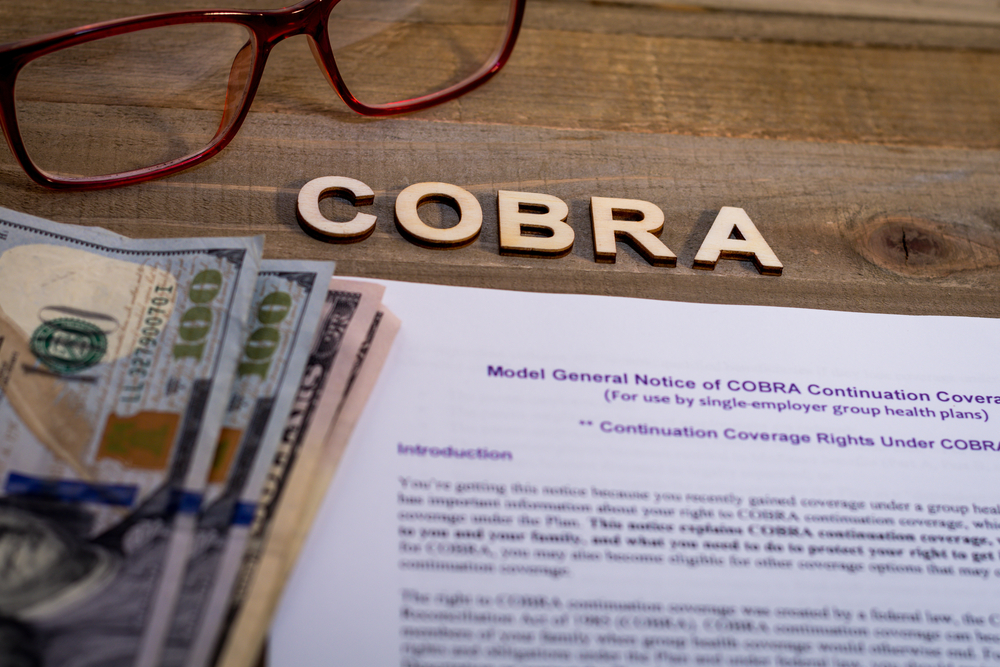
Employer COBRA Coverage
In the United States, the Consolidated Omnibus Budget Reconciliation Act (COBRA) allows employees to continue their existing workplace health insurance for a limited time after leaving employment, which can include transitioning to long-term disability.
While COBRA can be a lifeline for continuous coverage, it’s important to note that the individual is typically responsible for paying the full premium, which can be significantly higher without the employer’s contribution.
Planning and Communication
Effective planning and open communication with employers, insurance providers, and healthcare professionals are vital in navigating the coverage maze. Individuals should proactively engage in discussions about their insurance needs and options as soon as they anticipate a long-term disability.
The Bottom Line
Determining who pays for health insurance during long-term disability involves understanding the intersection of employer-provided benefits, private insurance policies, and government programs.
Each scenario presents its own set of rules and options, making it imperative for individuals to actively seek information and advice tailored to their specific situation.
Source: Read Full Article